Quick take: This guide shows you exactly How to Talk About STI Testing With Your Partner—when to bring it up, what to say, how to handle emotions, and what to do next (including results and prevention). You’ll get copy-paste conversation starters backed by leading health guidance, minus the shame. STIs are common and many have no symptoms; testing protects both of you and builds trust.
1) Why This Talk Matters
- STIs are common—and often symptom-free. Many infections don’t show symptoms, so you can’t rely on “feeling fine.” Screening protects both partners.
- Trust builder: Honesty about testing is relationship care, not mistrust.
- Stigma reducer: Talking openly normalizes sexual health and reduces shame.
2) Before You Start: Prep Yourself
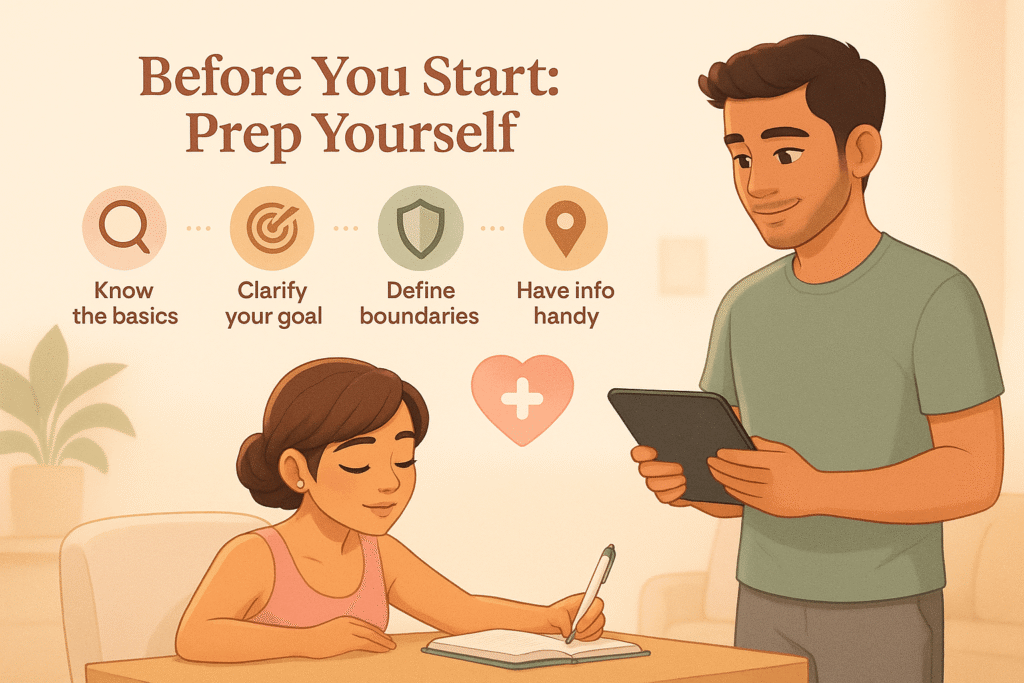
- Know the basics. Learn what to test for and how testing works (clinic or at-home).
- Clarify your goal. Example: “We’re becoming intimate; I want us tested so we both feel safe.”
- Define your boundaries. Decide what intimacy you’re comfortable with until results are shared.
- Have info handy. Know your local testing options.
3) Best Time & Place
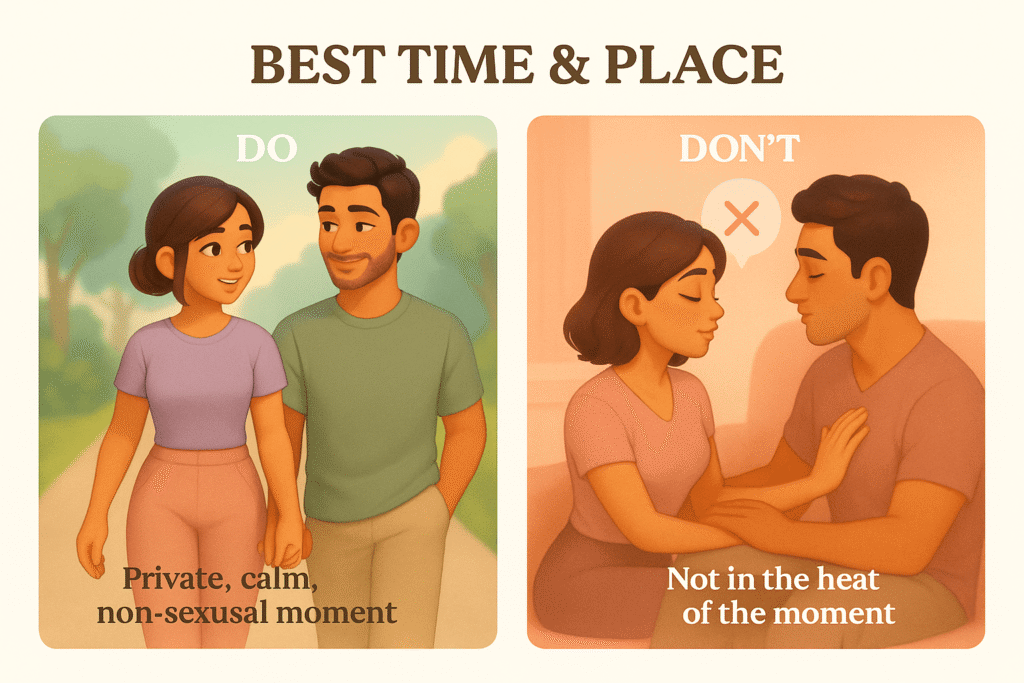
- Do: choose a private, calm, non-sexual moment (walk, coffee, quiet night in).
- Don’t: raise it in the heat of the moment.
- Tip: Talk before sex; suggest testing as a mutual act of care.
4) What to Say (Scripts You Can Copy)
- Mutual-care opener:
“I care about us and want to make sure we’re both healthy. Let’s get tested before we have sex—so we can look out for each other.” - Normalize & de-shame:
“A lot of STIs don’t have symptoms. Testing just gives us peace of mind.” - Lead by example:
“I was tested on [date]; happy to share my results. When was your last test?” - Suggest going together:
“Want to book an appointment together or order mail-in kits? We can make it easy.” - If they hesitate:
“No pressure—I know it can feel awkward. This is about caring for each other, not accusing.”
5) Handling Emotions & Stigma
- Validate feelings: “I get that this is uncomfortable. I feel a bit nervous, too.”
- Stay curious, not accusatory: “What would help you feel comfortable?”
- Reframe: “This is just routine health care—like a checkup.”
6) Talking About Results
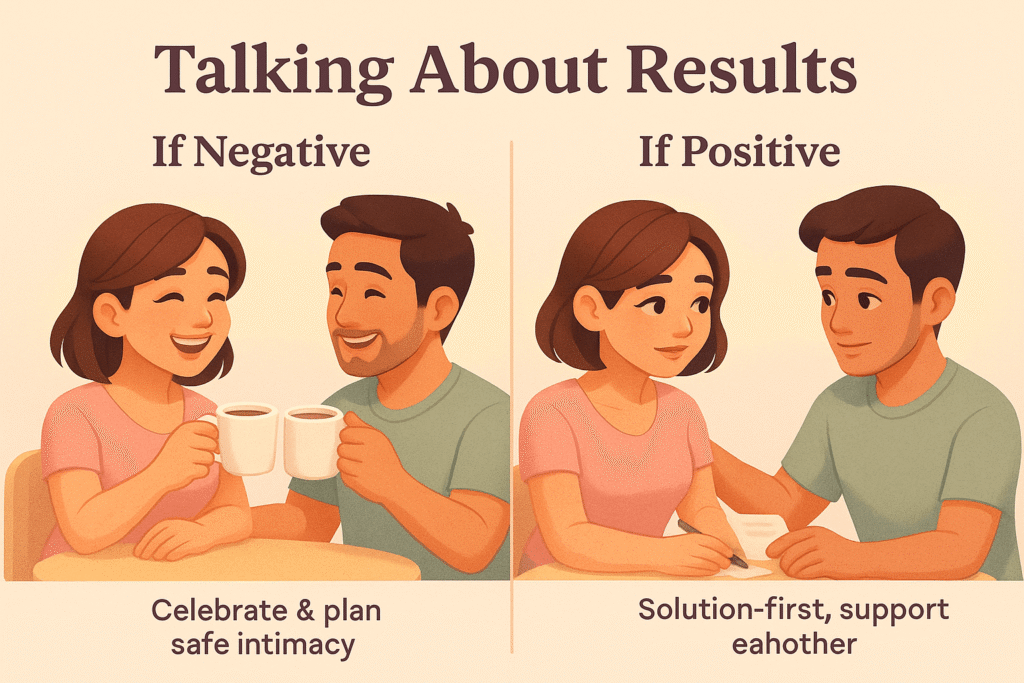
- Share before sex.
- If negative: celebrate, and discuss how to stay safe (condoms, barriers, testing schedule).
- If positive:
- Use a solution-first script:
“I tested positive for [infection]. It’s treatable/manageable; here’s my plan from the clinic. I want us to handle this together.” - Follow treatment guidance and support each other.
- Use a solution-first script:
7) Boundaries & Prevention
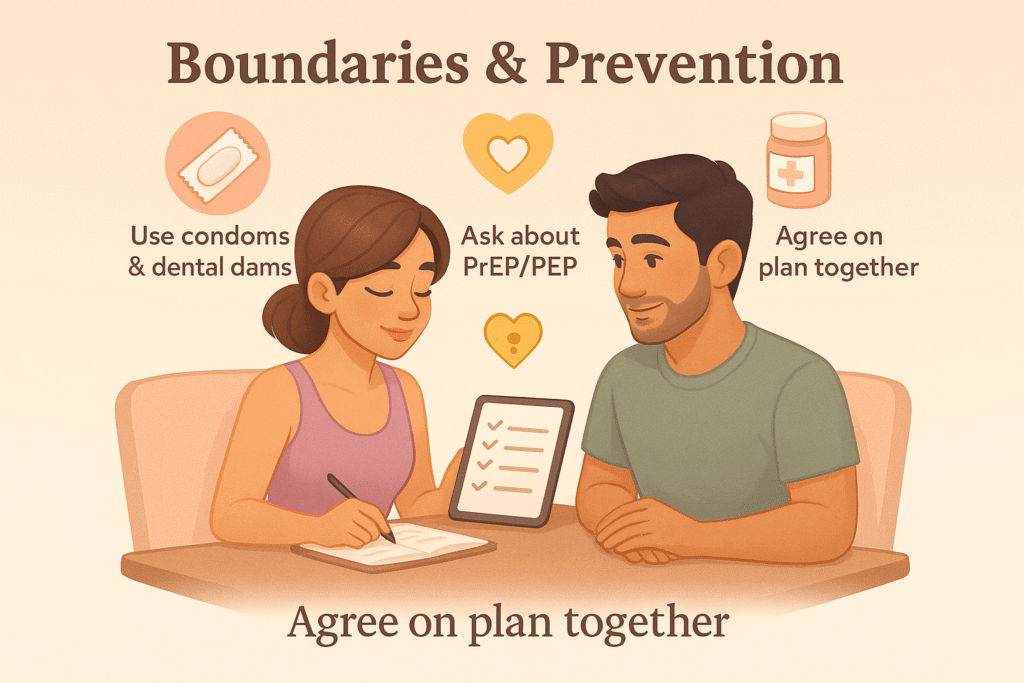
- Condoms and dental dams reduce risk.
- PrEP/PEP are options for HIV prevention—ask a clinician if relevant.
- Agree on a plan: “We’ll use protection until our results are in, then revisit.”
8) Keeping the Conversation Going

- Testing isn’t one-and-done. Make it part of your relationship routine.
- CDC guidance: every 6–12 months, or more often if you have multiple/new partners.
- Script:
“Let’s put testing on our calendar every [X] months so it stays easy and drama-free.”
9) Quick Checklist
- ☐ Pick a calm moment.
- ☐ Frame it as care, not suspicion.
- ☐ Share your last test date/results.
- ☐ Suggest going together or ordering kits.
- ☐ Set a temporary plan (barriers) until results.
- ☐ Schedule routine testing going forward.
10) FAQs
Stay calm. Explain why it matters, offer to test together, and set boundaries until you both feel safe.
Yes, at least once when becoming exclusive. After that, follow provider guidance.
Yes, mail-in lab kits are accurate for many STIs. Some infections require clinic testing.
Condoms, dental dams, and possibly PrEP (for HIV) if relevant.
Very. In the U.S., about 1 in 5 people had an STI at any given time in recent CDC estimates.
Final Word
Talking about STI testing is an act of respect and intimacy. Use the right timing, gentle scripts, and keep the conversation ongoing. When you treat sexual health like self-care, the fear fades—and intimacy grows stronger.




